door bhrw | jan 16, 2026 | B12, gezondheidszorg, wetenschap |

Scientists have identified the first DNA variant associated with a higher risk of developing B12 deficiency when a person is treated with metformin.
The analysis, which was done by the authors, identified a genome-wide non-synonymous SNP in the cubilin gene (CUBN, rs1801222/p.S253F), which was significantly associated with metformin-induced vitamin B12 deficiency. This finding was replicated in three Scottish cohorts, in the Diabetes Prevention Program Outcomes Study (DPPOS) cohort, and in a small clinical cohort from Liverpool. Vitamin B12 deficiency occurred in 0.84–1.20% of individuals who were not exposed to metformin regardless of their rs1801222 genotype. However, a large interaction with metformin use was observed, with vitamin B12 deficiency developing at 6.02% in GG, 7.96% in GA and 12.84% in AA genotype groups.
Co-author Ewan Pearson: “The 14% of white population with AA genotype are 2.5 times more likely to require B12 replacement GG. Equates to 10% requiring B12 replacement by 11 years after starting metformin with AA genotype vs 21 years for GG. A large effect!”
It should be noted that the primary analysis was conducted among participants in the UK Biobank. Individuals were identified with a diagnosis of vitamin B12 deficiency and/or a record of B12 injection prescriptions, and metformin use was extensively documented. However, clinical diagnosis of B12 deficiency is often only done on the basis of abnormal B12 measurements, and -for instance- measurements of methylmalonic acid are rarely done. Furthermore, people who are using (multi)vitamin supplementation may not so easily be recognized as truly B12-deficient. So, the incidence of B12 deficiency may be higher than reported in the paper. Nevertheless, this is great work in the beautiful dataset of UK Biobank, and confirmed in other cohorts, such as Generation Scotland, GoDARTS, and SHARE, and DPPOS. Researchers are eagerly awaiting the time when UK Biobank data will also be enriched with serum B12, MMA, and homocysteine measurements for all participants.
Full source: https://link.springer.com/article/10.1007/s00125-025-06655-5
door bhrw | dec 25, 2025 | AI, B12, gezondheidszorg |

In sommige discussiegroepen waar ik aan deelneem, komen soms hele lappen tekst voorbij, omdat één van de deelnemers aan ChatGPT een vraag heeft gesteld. Bijzonder is dat dit soort teksten nooit enige kritische reactie opleveren, en in de regel voor zoete koek worden aangenomen. Terwijl ook een AI systeem de plank ernstig mis kan slaan. Of bewust door zijn creatoren onjuist wordt geprogrammeerd.
Een paar voorvallen brachten mij er toe om een aantal AI systemen de zelfde vraag voor te leggen over de behandeling van pernicieuze anemie. Eén van die voorvallen was de volgende:
Dr. X. weigerde begin 2025 de B12 injecties voort te zetten bij een vrouw van midden 50, die al langer bekend was met auto-immuun gastritis, en die klachten had van pijnlijke neuropathie in de benen en voeten. Deze klachten waren nagenoeg geheel verdwenen door behandeling met frequente B12 injecties (2x per week 1000 mcg). De vrouw injecteerde zichzelf op dat moment 1x per 1.5 – 2 weken in de spier met hydroxocobalamine om klachtenvrij te blijven.
Een artikel in 2014 in het blad Huisarts & Wetenschap beschreef duidelijk dat tijdens B12 injectie behandeling de serum B12 waarde niet gecontroleerd dient te worden, omdat deze hoog hoort te zijn. Blijkbaar had dr. X. dit niet gelezen, want deze liet de B12 waarde wél controleren, en omdat die boven de 1476 pmol/l was (de bovengrens van de meetmethode) moest de onfortuinlijke vrouw haar B12 injecties direct staken.
De vraag die ik stelde aan de diverse AI systemen, was:
“A 50-year-old woman with pernicious anaemia is treated with a 1000 mcg B12 injection every two weeks, and due to this treatment, she is free of symptoms. How often should a doctor measure her serum B12 concentration?”
De antwoorden die deze vraag opleverde, en het volledige blog, vindt U hier:
https://pernicious-anaemia-society.org/blog/artificial-but-not-intelligent-asking-the-simplest-question/
door bhrw | dec 23, 2025 | B12, gezondheidszorg |

You may be selective in what you eat during the holidays. Some animals are less inclusive. For instance, this rat species mainly eats bamboo. An interesting study on diet and cardiovascular risk. This study explored the effects of vitamin B12 (VB12) supplementation on cardiovascular health in the silver star bamboo rat, a species that primarily feeds on bamboo. Bamboo-eating species like bamboo rats, giant pandas, and red pandas are at risk of VB12 deficiency, which can lead to elevated homocysteine levels and increased cardiovascular disease (CVD) risk.
The researchers first conducted a genome annotation of the bamboo rat to enable evolutionary studies. Comparative transcriptomics revealed that bamboo rats had upregulated genes associated with CVD, indicating higher disease risk compared to carnivorous and omnivorous rodents.

After 60 days of VB12 supplementation, liver transcriptome analysis showed significant improvements in cardiovascular health markers. VB12 led to reduced cholesterol synthesis, enhanced fatty acid metabolism, decreased homocysteine levels, lower LDL-to-HDL ratios, and increased apolipoprotein A-to-apolipoprotein B ratios. These findings suggest that VB12 supplementation can help mitigate CVD risk in bamboo-eating species.
On a related note:
One of the phenomena that is often observed around the holiday season is the rise in cardiovascular-based mortality, commonly referred to as the “Christmas Holiday Effect.” This trend has been observed in the United States and worldwide, including Norway, Sweden, Canada, and Denmark. Despite the festive spirit that surrounds this time of year, research consistently shows that cardiovascular deaths spike between late December and early January.
The numbers are striking. A 2016 study published in the Journal of the American Heart Association found that cardiac events increased by 4.2% between December 25 and January 7. One of the earliest hypotheses was that the colder weather experienced in the northern hemisphere during this period might be a major contributor. However, researchers found the same effect in New Zealand, a country experiencing summer during this time. This indicates that other factors beyond climate are at play.
Source: https://www.elliothospital.org/about-us/newsroom/news/holiday-heart-attack-phenomenon-and-how-avoid-it
What will you do to mitigate Christmas-dinner-associated cardiovascular risk?
This blog appeared in CluB-12’s December 2025 Newsletter.
door bhrw | nov 12, 2025 | B12, gezondheidszorg |
De laatste paar jaar zien we steeds meer onderzoekingen naar de relatie tussen vitamine B12 en cognitief functioneren op oudere leeftijd. Onderstaande artikel beschrijft een heel mooi en gedegen onderzoek op dit gebied.

Dit artikel van Francesca Marino en collega’s beschrijft een groot onderzoek naar de rol van vitamine B12 in het behoud van cognitieve functies (zoals geheugen, taal en plannen) bij oudere mensen. De onderzoekers wilden weten of mensen die vanaf middelbare leeftijd tot op oudere leeftijd een betere vitamine B12-status hebben, minder snel achteruitgaan in hun denken en geheugen dan mensen met een lage B12-status.
Mede-auteurs Josh Miller en Jacob Selhub zijn bekende onderzoekers op het gebied van de B12 stofwisseling, en o.a. lid van CluB-12 (https://www.club-12.org).
De bevolking veroudert en dementie komt steeds vaker voor. Hoewel dementie niet te genezen is, weten we dat sommige (leefstijl)factoren de kans op cognitieve achteruitgang kunnen beïnvloeden. Eerder onderzoek naar de relatie tussen B12 en cognitief functioneren leverde tegenstrijdige resultaten op. Een belangrijk probleem is dat veel studies B12 slechts één keer meten, of alleen vragen naar voeding, wat onnauwkeurig kan zijn. Ook de bloedwaarde van B12 geeft niet altijd een goed beeld: iemand kan een “normale” B12 hebben terwijl de cellen toch te weinig B12 krijgen of kunnen opnemen uit het bloed. Daarom gebruikten de onderzoekers in dit onderzoek een combinatie-indicator, de 3cB12 indicator, die drie biomarkers samenvoegt: vitamine B12, methylmalonzuur (MMA) en homocysteïne (Hcy). Ook al weten we dat bij B12 tekort de biomarkers MMA en Hcy niet altijd verhoogd zijn, toch geeft dit een veel betrouwbaarder beeld van de balans in de B12 stofwisseling.
(meer…)
door bhrw | okt 17, 2025 | Geen categorie |
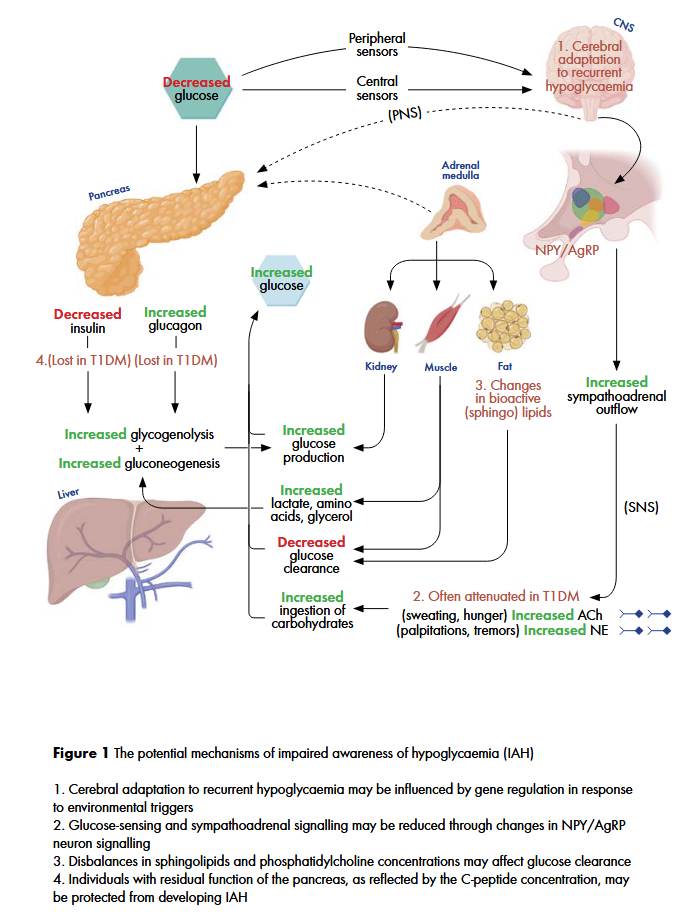
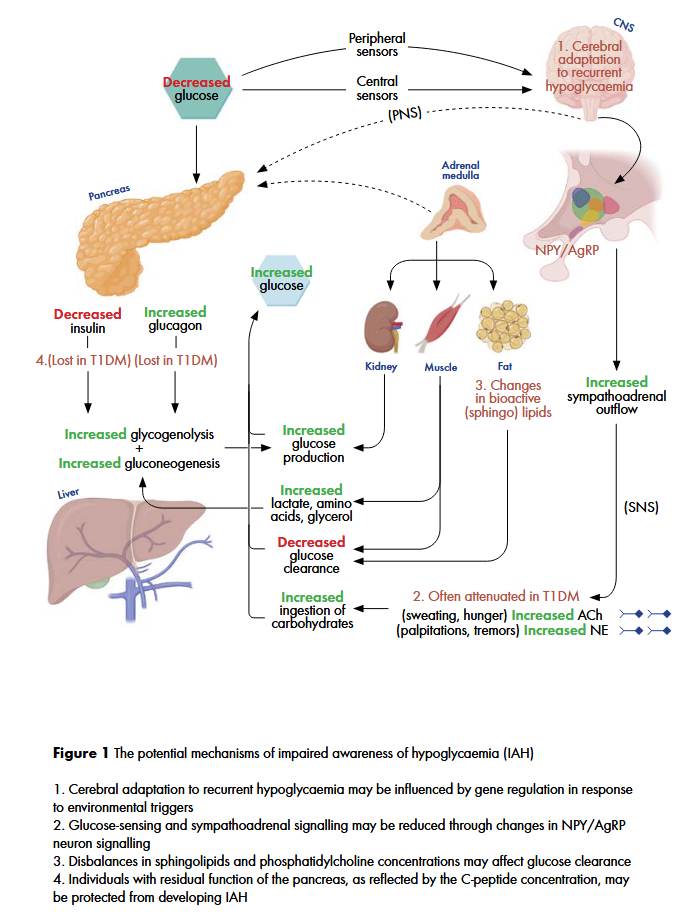
The title of this blog contains two abbreviations, but important ones. IAH is impaired awareness of hypoglycaemia, and AGRP (or AgRP) is agouti-related protein. They are central in a paper just published by my talented colleague, Dr. Rita Varkevisser.
Learn how she summarizes the importance of this paper:
A compelling finding of this study was the association between agouti-related protein (AgRP) and impaired awareness of hypoglycaemia. AgRP is an important neuropeptide in energy homeostasis and is expressed in the adrenal gland and hypothalamus, specifically in the arcuate nucleus (ARC) and ventral hypothalamic nucleus (VMH) where central glucose sensing occurs. These glucose-sensing neurons in the ARC can influence glucose homeostasis through the activation of the autonomic nervous system and exert orexigenic effects through release of AgRP which inhibits MC4R neurons that stimulates food intake. The lower circulating plasma AgRP in individuals with IAH could suggest that these individuals could be less responsive to lower glucose levels. This may be due to threshold changes in the glucose-sensing neurons in the ARC and less hypothalamic-pituitary-adrenal (HPA) activation leading to less AgRP release from neuroendocrine cells in the adrenal medulla.
Another mechanism that may reduce AgRP release is the inhibition by other hormones such as insulin and leptin. Higher circulating levels of insulin usually leads to a reduction in appetite. In some individuals, hypothalamic insulin resistance may lead to increased food consumption despite higher circulating insulin levels. As a consequence of this insulin resistance, these individuals may be protected from hypoglycaemia, as the appetite suppression that would normally occur is no longer present. Although it is not yet clear how recurrent hypoglycaemia can influence glucose sensing and ARC/VMH mediated counterregulatory responses, further research into AgRP may help to elucidate the pathophysiology of IAH.
The mechanisms which dr. Varkevisser summarizers to play a role in IAH, are shown in this figure:
Dr. Varkevisser successfully defended her scientific thesis in November 2024. The full thesis with all her articles can be found on the University of Groningen website: https://research.rug.nl/en/publications/a-balancing-act-navigating-cardiovascular-vigilance-and-hypoglyca
door bhrw | sep 28, 2025 | AGEs, diabetes, gezondheidszorg |

John Mulder, CEO of Diagnoptics: “Mid September, a Dutch national newspaper devoted a full-page article to biological age and AGEs. It’s striking to see how a topic that once lived only in research papers and specialist discussions is now reaching a much wider audience.
Public awareness of biological age is clearly growing, not only among scientists and clinicians, but also within society at large. This raises an important question for all of us in the medical field: how do we translate this momentum into clinical practice?
AGEs remain underexplored in everyday healthcare. Yet early findings already suggest they can add value in prevention, patient engagement, and even perioperative decision-making. For me, this underscores the importance of bridging science and practice, ensuring that what we measure can truly drive better care.
Bron: LinkedIn
(meer…)













Recente reacties